Glaucoma
What is glaucoma?
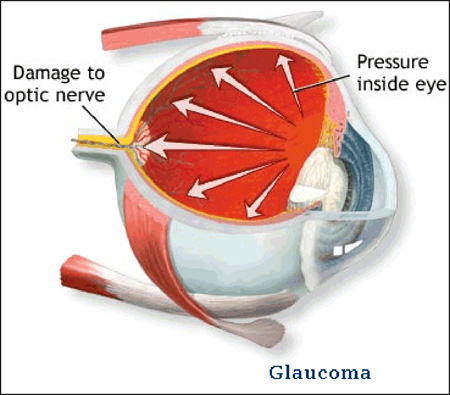 Glaucoma is an eye disease in which the optic nerve is damaged in a characteristic pattern. This can permanently damage vision in the affected eye(s) and lead to blindness if left untreated. It is normally associated with increased fluid pressure in the eye (aqueous humour). The term “ocular hypertension” is used for people with consistently raised intraocular pressure (IOP) without any associated optic nerve damage. Conversely, the term ‘normal tension’ or ‘low tension’ glaucoma is used for those with optic nerve damage and associated visual field loss, but normal or low IOP.
Glaucoma is an eye disease in which the optic nerve is damaged in a characteristic pattern. This can permanently damage vision in the affected eye(s) and lead to blindness if left untreated. It is normally associated with increased fluid pressure in the eye (aqueous humour). The term “ocular hypertension” is used for people with consistently raised intraocular pressure (IOP) without any associated optic nerve damage. Conversely, the term ‘normal tension’ or ‘low tension’ glaucoma is used for those with optic nerve damage and associated visual field loss, but normal or low IOP.
Glaucoma: What is the optic nerve?
The optic nerve is made up of over 1.2 million axons (individual nerve fibers). It serves as a relay between the retina and the brain. The retina absorbs the external light waves and transmits them via the optic nerve to the brain.
What are the different forms of glaucoma?
- Childhood (Congential)
- Open-Angle Glaucoma
- Angle Closure Glaucoma
Primary Open Angle Glaucoma is the 2nd leading cause of blindness in the US.
The most common form of glaucoma is primary open-angle glaucoma. However there are other types including congential glaucoma,low tension glaucoma, angle closure glaucoma, and the broad category of secondary glaucomas. Secondary glaucoma includes for example: pigmentary glaucoma, neovascular glaucoma and steroid induced glaucoma.
How does glaucoma cause vision loss?
glaucoma initially causes no symptoms, but loss of side vision (peripheral vision)

What are the symptoms of glaucoma?
- no symptoms
- visual field defects
- blurred vision
- colored halos around lights
- pain
- red eye
- vomiting
- headache
Risk Factors for glaucoma?
Racial Background
- Inuit Population have 20-40x prevalence of primary angle closure glaucoma compared to the white population in the US.
- Asian Population have higher rates of primary angle closure glaucoma.
- Black Population are 3-4x more likely than whites to have glaucoma (Baltimore Eye Study) African Ancestry
- Hispanic/Latino Ancestry (Los Angeles Latino Eye Study (LALES)
Gender Acute angle closure glaucoma has been reported more often in women than men. Studies have shown that women have more shallow anterior chambers than men.
Age The anterior chamber decreases in depth and volume with age. These changes predispose to papillary block.
- Prevalence of glaucoma among whites was 3.5x higher for individuals in their 70s than in their 40s (Baltimore Eye Survey)
Refraction
- Hyperopia (patients with nanophthalmos with small eyes and smaller anterior chamber)
- Myopia
Inheritance (Genetics) Congenital (CYP1B1 gene); positive Family history (TIGR/myocilin gene (MYOC)on chromosome 1)
Increased Cup to Disc Ratio
Thinner Central Corneal Thickness (< 550um)
Other factors may include: diabetes mellitus Type 2, myopia, hypertension, migranes, trauma, sickle cell disease, uveitis, corticosteroid use, post retinal detachment, intraocular tumors, retinal or ocular ischemia(i.e. vein occlusions)
What can I do to protect my vision?
Important to have a complete eye examination for early detection and thus optimize and preserve vision.
Recommend: An annual eye examination every two years prior to age 40 and annual after age 40.
The American Academy of Ophthalmology (AAO) recommends screening for glaucoma as part of the comprehensive adult medical eye evaluation, starting at the age of 20, with a frequency depending on an individual’s age and other risk factors for glaucoma.
How is glaucoma detected?
- Clinical examination (Ophthalmoscopy)
- Goniscopy (examination of the angle structures with a special lens)
- Intraocular Pressure(IOP) Measurement (Normal range is 10-21mmHg)
- Ocular Coherence Tomography (OCT) of optic nerve &retinal nerve fiber layer (rNFL)
- Corneal Pachymetry
- Visual Field Testing
How is glaucoma treated?
- Congenital Glaucoma:
Primary treatment is surgical and may also require topical medications
- Adult Onset Glaucoma:
Primary treatment: Pharmacologic (Medications:Topical Eye Drops)
Laser Treatment (i.e. Selective Laser Trabeculoplasty, Laser Iridotomy)
Cyclophotocoagulation: laser treatment of the ciliary body
Surgery: Surgical Iridectomy,Trabeculetomy/Drainage Implants(Setons/Tubes)
At the Massachusetts Eye Research and Surgery Institution (MERSI) we are using the latest and most sensitive technology to monitor the optic nerve in an effort to preserve vision as well as cutting edge treatment modalities.
What are the complications of uveitis?
- Vision loss
- Cataracts
- Glaucoma
- Macular edema
- Retinal detachment
- Hypotony (low pressure in the eye)
- Blood vessel damage
- Scarring of the cornea (band keratopathy) retina, or choroid
Vision loss is the number one complication of uveitis. Uveitis is the third leading cause of preventable blindness worldwide. This can be secondary to several other complications listed above. Some of these can be treated, but damage can become permanent.
Also, in treating uveitis, corticosteroids can lead to their own set of complications. This is why it is vital that inflammation be treated aggressively before these complications occur, and without long term dependence on corticosteroids.
Our Physicians
All of our physicians have completed Fellowships in their specialty.
C. Stephen Foster, MD, FACS, FACR
Founder
Stephen D. Anesi, MD, FACS
Partner and Co-President
Peter Y. Chang, MD, FACS
Partner and Co-President
Peter L. Lou, MD
Associate
